ABRAXANE and Advanced Pancreatic Cancer
What should I know about advanced pancreatic cancer?
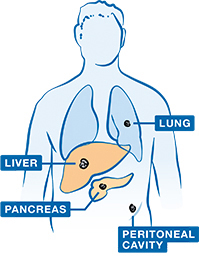
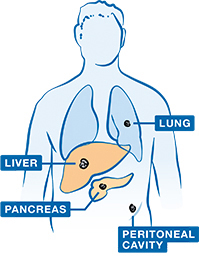
Most common places in the body where advanced pafncreatic cancer may spread.
What is advanced pancreatic cancer?
Pancreatic cancer is cancer that starts in the pancreas (PAN-kree-uhs). The pancreas is an organ found behind your stomach. It does 2 important things in the body:
- Makes enzymes (chemicals) that help the body digest food
- Makes hormones (chemicals) that regulate the amount of sugar in your blood
Pancreatic cancer happens when abnormal cells in the pancreas grow out of control and form a tumor (TOO-mer). A tumor is an abnormal mass of tissue.
When the cancer spreads from the pancreas to other parts of the body it is called advanced pancreatic cancer. This type of cancer is also known as metastatic (met-tuh-STA-tik) or stage 4 pancreatic cancer.
Most common places in the body where advanced pancreatic cancer may spread.
How many people have advanced pancreatic cancer?
If you have advanced pancreatic cancer, you are not alone. Nearly 26,000 people in the United States are diagnosed each year with this type of cancer.
Are some people more at risk for pancreatic cancer?
There are certain factors that affect a person’s chance of getting pancreatic cancer. It is important to know that having 1 or more risk factors does not mean that you will definitely get pancreatic cancer. And some people may get this type of cancer even if they don’t have any risk factors.
In addition to a person’s age, gender, race, and family history—all things that can’t be changed—there are risk factors for pancreatic cancer that are considered lifestyle factors. This means that they can be controlled to some degree.
What is important to know about diet and nutrition?
When you or your loved one were diagnosed with advanced pancreatic cancer, your doctor or healthcare team may have talked to you about the importance of good diet and nutrition. This is because the pancreas plays a key role in digestion:
- The pancreas produces certain enzymes (chemicals) that help break down food as well as hormones that regulate the amount of sugar in your blood
- Pancreatic cancer can change how the pancreas makes these enzymes and hormones. As a result, digestion—the ability to take up nutrients from food—and regulation of blood sugar are affected
- Surgery to remove all or part of the pancreas can also affect the levels of enzymes and hormones produced
Eating can become challenging when you are living with pancreatic cancer. Developing a healthy eating plan—with the help of your doctor or nutritionist—is important and may help you to better manage your symptoms.
Before making any changes to your diet or adding any supplements, it is important to talk to your doctor or nutritionist. Here are some tips that your doctor may suggest:

- Eat small meals more often throughout the day. Try to eat a little bit of food every 4 hours and include protein as much as you can
- Have foods and drinks separately. Waiting 20 minutes before or after meals to have a beverage helps prevent nausea and keeps you from filling up on empty calories
- Eat slowly. This helps you digest better so you don’t feel uncomfortable
- Keep a food diary. A food diary may help you keep track of how you feel after eating different foods so that you can be aware of which ones to avoid
- Talk to your doctor. Be sure to ask your doctor about how best to meet your nutritional needs. It may also help to speak to a nutritionist or dietitian

What are some tips for improving my appetite?
You may notice that your appetite has changed as a result of your cancer. This may happen because foods start to taste different to you or because you just don’t feel as hungry as you used to. It is important to try to improve your appetite so that you can get the proper nutrition you need. Here are some tips your doctor may suggest:
- Get plenty of rest
- Do light exercise before meals
- Choose foods that you like and that smell good
- Plan your meals a day ahead of time
- Drink 8 to 12 cups of clear liquids a day so you stay hydrated
- Try to eat 6 to 8 small meals and snacks a day, especially at those times when you are most hungry
- Eat at scheduled times, even if you aren’t hungry
- Replace a meal with a supplement drink or smoothie made with protein powder. If your doctor has prescribed pancreatic enzymes, take them with these drinks
- Keep small bowls of healthy snacks around the house so you can eat them between meals. Nuts and fruits are good choices
- Take antinausea medicines when you first start to feel sick to your stomach. Put off eating your favorite foods if you feel nauseous
- Arrange your foods so they look attractive. You may choose foods of different colors or use lemons or limes as garnishes
- Make your mealtimes pleasing by using colorful place settings, watching a favorite TV show as you eat, or playing music
- Put small portions of food on large plates to help it seem less overwhelming
If your appetite remains low, or you start or continue to lose weight, be sure to talk to your doctor. He or she may prescribe medicine to help boost your appetite.
This information is for educational purposes only. It is not meant to replace the advice of a healthcare provider. Always consult with a doctor or other healthcare provider regarding your or your loved one’s medical needs.
For more information and tips on pancreatic cancer and nutrition, visit the Pancreatic Cancer Action Network (PanCAN®) website at .
What is ABRAXANE?
ABRAXANE is a prescription medicine used to treat advanced pancreatic cancer, when used in combination with gemcitabine (jem-CY-tuh-been), as the first medicine you receive for advanced pancreatic cancer.
ABRAXANE is a chemotherapy (KEE-moh-THAYR-uh-pee). Chemotherapy is a type of medicine that is used to keep cancer cells from growing or to kill cancer cells. Treatment with ABRAXANE and gemcitabine may help control or slow the spread of cancer cells.
Your doctor may recommend treatment with ABRAXANE + gemcitabine based on the stage of your cancer and your overall health. Only your doctor can help you decide if ABRAXANE + gemcitabine is right for you.
What is in ABRAXANE?
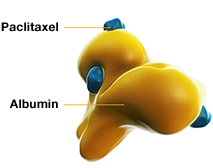
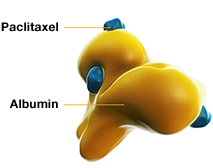
The medicine in ABRAXANE, paclitaxel, is bound to albumin.
Illustrative purposes only.
ABRAXANE is a different formulation of the cancer-fighting medicine paclitaxel (PAK-li-TAK-sel). ABRAXANE is made by binding paclitaxel to albumin (al-BYOO-min). Albumin is a protein found in the blood.
The medicine in ABRAXANE, paclitaxel, is bound to albumin.
Illustrative purposes only.
Here is what this means to you:
- Because ABRAXANE is bound to albumin, no solvents are needed to dissolve it
- Solvents are chemicals that dissolve some medicines so that they can be given by infusion (in-FYOO-zhun)
- Some solvents can cause allergic reactions
- Since ABRAXANE does not contain solvents, it is not usually necessary to take medicines to prevent allergic reactions before ABRAXANE is given. These medicines are called premedication
It is important to know that allergic reactions can occur with ABRAXANE. Premedication may be needed if you have had an allergic reaction. Allergic reactions may be severe and can lead to death. In case of severe allergic reaction, ABRAXANE should not be used again.
How does ABRAXANE work?

ABRAXANE travels through the bloodstream to reach cells in many parts of the body, including cancer cells.
Illustrative purposes only.
ABRAXANE may help stop cancer cells from dividing and making new cells. ABRAXANE works by blocking the action of proteins called microtubules (MY-kroh-TOO-byools). These proteins help cells divide.
Systemic (sis-TEH-mik) treatments like ABRAXANE are used to treat metastatic (meh-tuh-STA-tik) cancer. This is cancer that has spread from one part of the body to another. It is also known as advanced or stage 4 cancer. Systemic treatments travel through the bloodstream. This makes it possible to reach cells in many parts of the body, including cancer cells. ABRAXANE may also affect normal cells. This may cause side effects.
ABRAXANE travels through the bloodstream to reach cells in many parts of the body, including cancer cells.
Illustrative purposes only.

How are ABRAXANE and gemcitabine given?
ABRAXANE and gemcitabine are given by intravenous (IN-truh-VEE-nus), or IV, infusion (in-FYOO-zhun). Both medicines are given at the same visit. To begin the infusion
- A nurse inserts a thin, soft tube into your vein to give the medicine. This is often called an IV. If you have a central line in place, the nurse will use that to give you the medicine
- The first medicine, ABRAXANE, flows through the IV into your bloodstream
- The second medicine, gemcitabine, is given right after ABRAXANE
- After each infusion, the nurse removes the IV or the device that delivered the medicine through your central line. Your central line or port stays in place
Treatment with ABRAXANE can cause irritation where the medicine is injected (injection site reactions). You should be monitored by your doctor or nurse during and after you receive ABRAXANE to make sure no problems occur at the injection site. In some cases, these problems occurred 7 to 10 days after the medicine was injected.
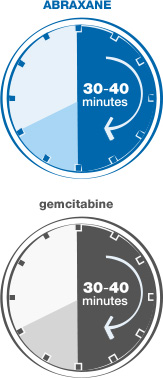
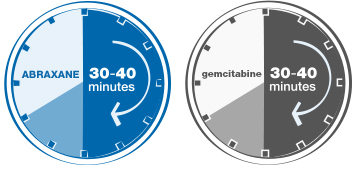
Your treatment with ABRAXANE + gemcitabine will be given in your doctor’s office, at a hospital, or at an infusion center. Each infusion of ABRAXANE takes 30-40 minutes. Gemcitabine infusion also takes about 30-40 minutes. Tests, checkups, or waiting time may affect the length of treatment sessions.
How often will I be given ABRAXANE + gemcitabine?
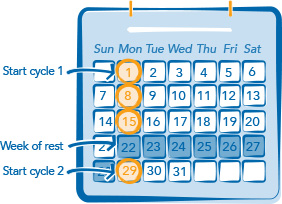
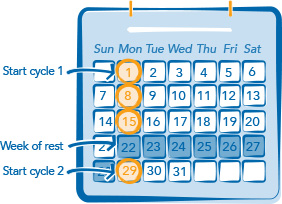
ABRAXANE is given once a week for 3 weeks in a row, on days 1, 8, and 15.
- Gemcitabine (jem-CY-tuh-been) is given right after ABRAXANE during the same visit
- After 3 weeks of treatment, you will get 1 week of rest. This 4-week period is called a treatment cycle
Your doctor will decide how many cycles you will get.
What results were seen in a study with ABRAXANE + gemcitabine?
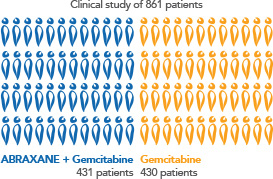
A clinical study of 861 patients with advanced pancreatic cancer looked at
- How well ABRAXANE + gemcitabine (jem-CY-tuh-been) worked
- The safety of ABRAXANE + gemcitabine
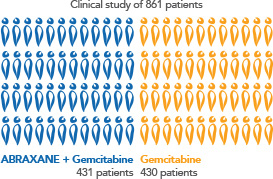
ABRAXANE + gemcitabine was given to 431 patients, and 430 patients received only gemcitabine. Both groups of patients were given these medicines as their first treatment for advanced pancreatic cancer.
ABRAXANE + gemcitabine helped some patients live longer.
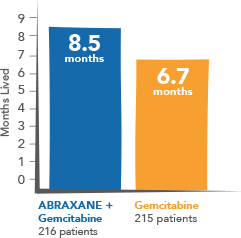
Results from this study showed that some patients who were given ABRAXANE + gemcitabine lived longer than patients given only gemcitabine:
- Half of the 431 patients given ABRAXANE + gemcitabine lived 8.5 months or longer
- Half of the 430 patients given gemcitabine alone lived 6.7 months or longer
A standard way of assessing cancer treatments in a clinical study is to measure how long the patients in each group live.



